Stages of Diabetic Foot Ulcer | 5 Stages, Signs & Treatment
A diabetic foot ulcer is one of the most serious complications of diabetes and a major cause of hospitalization among diabetic patients. High blood sugar affects nerves, blood circulation, and the body’s ability to heal, making the feet extremely vulnerable to injury, infection, and tissue breakdown.
Early recognition of the stages of diabetic foot ulcer is essential for preventing complications such as deep infections, bone involvement, and even amputation. With timely care from an experienced vascular specialist like Dr. Santosh Patil, patients can achieve faster healing, reduced recurrence, and improved quality of life.
In this patient-focused article, we discuss the 5 stages of diabetic foot ulcer, early signs to identify, and modern treatment options available today.
What Is a Diabetic Foot Ulcer?
A diabetic foot ulcer is an open wound that forms on the foot due to a combination of factors such as:
- Peripheral neuropathy (nerve damage)
- Peripheral artery disease (PAD)
- Poor blood flow
- High blood sugar levels
- Foot deformities or calluses
- Infection or trauma
These ulcers commonly appear on the bottom of the foot, toes, or pressure points, and they may progress rapidly if the underlying cause is not treated.
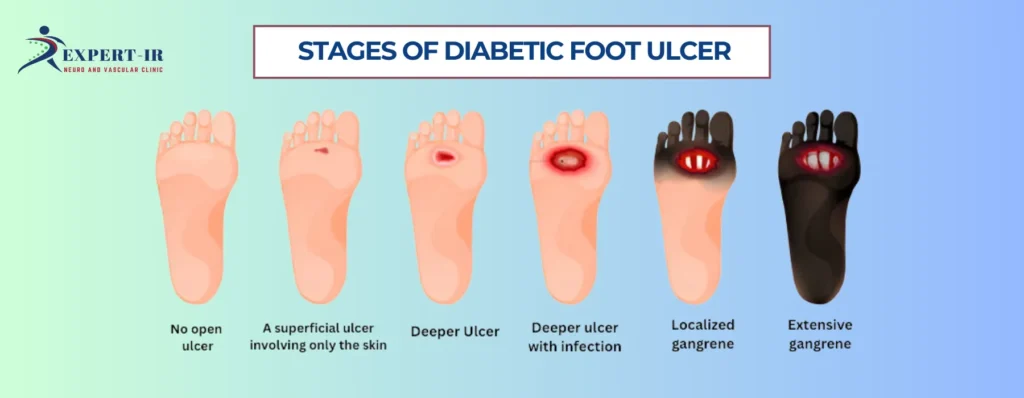
5 Stages of Diabetic Foot Ulcer
Diabetic foot ulcers progress through distinct stages. Understanding these stages helps patients monitor healing, recognize danger signs early, and seek expert care immediately.
Stage 1: Callus Formation and Skin Breakdown
The earliest sign of a diabetic ulcer is the formation of a callus or thickened skin. Due to neuropathy, patients may not feel pressure or friction, causing repetitive stress that leads to:
- Hard skin
- Redness
- Warm patches
- Minor cracks
- Loss of sensation
This stage is often ignored, but catching it early is crucial. Without intervention, calluses create pressure points that break down into open wounds.
Dr. Santosh Patil emphasizes regular foot checks for diabetic patients, as early detection prevents ulcer progression.
Stage 2: Superficial Ulcer Formation
At this stage, an open sore develops. The ulcer affects only the upper layers of the skin (epidermis and dermis). Signs include:
- Shallow wound
- Clear or red discharge
- Local swelling
- Mild odor
- Mild pain (or no pain due to neuropathy)
Although this stage is not deep, infection risk is high. Immediate cleaning, dressing, and medical evaluation are necessary.
Stage 3: Deep Ulcer Extending Into Muscles and Tendons
If untreated, the ulcer becomes deeper and may extend into:
- Subcutaneous tissue
- Muscles
- Tendons
Patients may notice:
- Increased discharge
- Visible yellow or necrotic tissue
- Worsening odor
- Swelling and redness
- Warm skin indicating infection
This stage often involves bacterial growth and requires urgent vascular evaluation, antibiotic therapy, and wound care.
Stage 4: Abscess or Bone Infection (Osteomyelitis)
At this serious stage, the infection spreads beyond soft tissue and may reach:
- Bone
- Joints
- Deep fascia
Symptoms become more severe:
- Intense swelling
- Fever
- Pus formation
- Severe odor
- Difficulty walking
- Increased blood sugar levels due to infection
Deep ulcers with bone involvement require advanced medical care, imaging tests, and often minimally invasive vascular procedures to restore blood flow.
Stage 5: Gangrene and Tissue Death
This is the most critical stage. The ulcer results in tissue death due to:
- Complete loss of blood supply
- Severe infection
- Extensive tissue damage
Symptoms include:
- Blackened skin
- Severe odor
- Numbness
- Cold limb
- Visible tissue death
Gangrene is a medical emergency. Immediate vascular intervention is necessary to restore circulation and prevent limb loss.
Dr. Santosh Patil, as a leading vascular surgeon in Pune, specializes in rapid diagnosis, revascularization procedures, and limb-saving treatment strategies.
Signs of a Diabetic Foot Ulcer You Should Never Ignore
Patients with diabetes should seek prompt medical care if they notice any of these symptoms:
- Persistent redness, swelling, or warmth
- Hard skin or callus
- Open wound on toes or foot
- Discoloration
- Tingling or numbness
- Drainage or bad odor
- Foot pain (or loss of pain due to neuropathy)
- Difficulty walking
How Diabetic Foot Ulcers Are Diagnosed
At Dr. Santosh Patil’s Vascular Clinic in Pune, diagnosis includes:
- Detailed foot examination
- Doppler ultrasound (to assess blood flow)
- X-ray or MRI (to detect bone infection)
- Lab tests for infection
- Ankle-Brachial Index (ABI)
- Blood sugar and vascular evaluation
Accurate diagnosis ensures proper treatment planning and faster healing.
Treatment for Diabetic Foot Ulcers
1. Restoring Blood Flow (Revascularization)
If poor circulation is the root cause, restoring blood flow is essential. Treatments include:
Angioplasty and Stenting
A catheter with a balloon is inserted into the artery to open blockages and improve blood flow.
Bypass Surgery
Creates a new path for blood to reach the foot.
Restoring circulation helps the ulcer heal faster and reduces recurrence.
2. Wound Care Management
Effective wound care includes:
- Cleaning the wound
- Removing dead tissue (debridement)
- Specialized dressings
- Moist wound healing techniques
- Offloading pressure from the foot
Advanced dressings help protect the wound and speed up healing.
3. Infection Control
Antibiotics are required when infection is present. In severe cases, hospitalization may be necessary.
4. Blood Sugar Management
High sugar levels slow healing and fuel infections. Proper diabetic control is essential for ulcer recovery.
5. Offloading Techniques
Reduces pressure from the ulcer site using:
- Special footwear
- Casts
- Insoles
- Walking boots
These devices help wounds heal faster by minimizing friction and pressure.
6. Lifestyle and Foot Care Tips
Patients are advised to:
- Check their feet daily
- Wear proper footwear
- Keep feet clean and dry
- Avoid walking barefoot
- Stop smoking
- Maintain healthy blood sugar levels
These habits prevent re-ulceration.
Dr. Santosh Patil, known as the Best Vascular Surgeon in Pune, brings extensive experience in diagnosing and treating diabetic foot conditions. His expertise includes:
- Advanced vascular imaging
- Minimally invasive revascularization
- Limb-saving interventions
- Personalized wound care plans
- Long-term ulcer prevention strategies
His patient-centric approach ensures compassionate care, accurate diagnosis, and successful outcomes.
Frequently Asked Questions (FAQs)
Early signs include redness, callus formation, swelling, hard skin, minor cracks, or drainage. Patients may also experience numbness due to nerve damage. Detecting these symptoms early can prevent ulcer progression.
Diabetic ulcers progress from callus formation → superficial ulcer → deep ulcer → infection or abscess → gangrene or tissue death. Identifying the correct stage helps guide treatment effectively.
Slow healing occurs due to poor blood flow, high blood sugar, nerve damage, and weak immune response. Without restoring circulation and controlling diabetes, healing remains incomplete or delayed.
Treatment involves wound cleaning, debridement, advanced dressings, blood sugar control, infection management, pressure offloading, and restoring blood flow through angioplasty or bypass. Dr. Santosh Patil – Best Vascular Surgeon in Pune specializes in these advanced vascular treatments.
Yes. Prevention includes daily foot inspections, wearing proper footwear, controlling blood sugar, avoiding walking barefoot, moisturizing the feet, and maintaining good circulation through regular activity.
Conclusion
A diabetic foot ulcer is a warning sign that requires immediate medical attention. Understanding the 5 stages of diabetic ulcer progression helps patients take control of their foot health and prevent severe complications like infection, hospitalization, or amputation.
With modern diagnostics and advanced vascular treatments available at Dr. Santosh Patil’s clinic, patients can achieve faster healing, improved mobility, and long-lasting relief.
If you have diabetes, never ignore changes in your feet—early intervention saves limbs and lives.