Can Varicocele Cause Low Sperm Count? Expert Insights
Male infertility is more common than many people realize, and in a significant number of cases, the cause is treatable when identified early. One condition that frequently raises concern among men trying to conceive is varicocele. Many patients ask a crucial question: Can varicocele cause low sperm count? The short answer is yes—but the full explanation is far more nuanced and important for long-term reproductive health.
This blog offers expert, evidence-based insights into how varicocele affects sperm count, sperm quality, and fertility, while also explaining when treatment becomes necessary and what modern, non-surgical options are available.
How Varicocele Affects Sperm Production
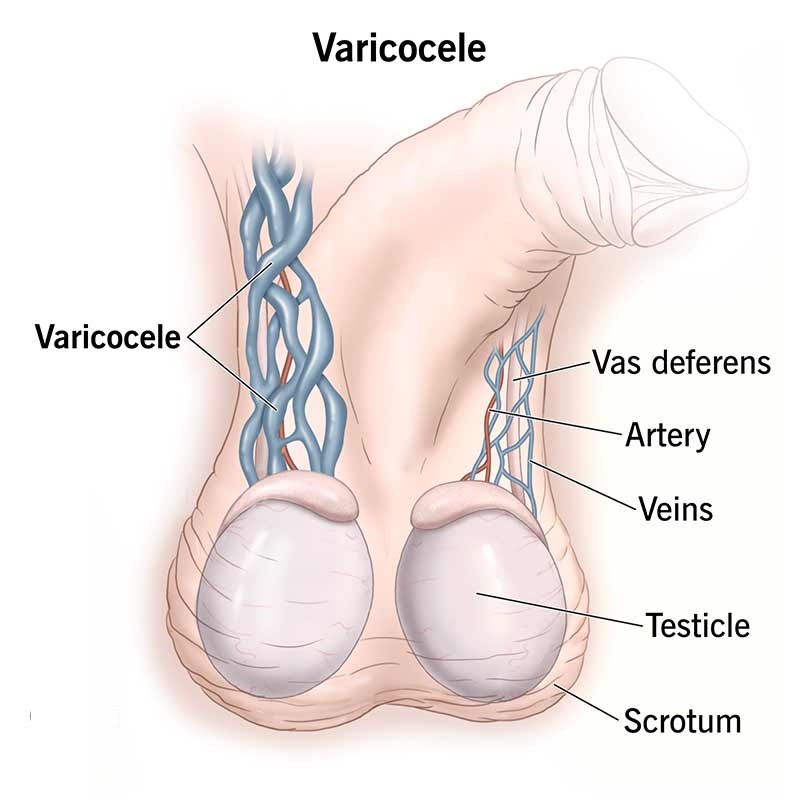
The testicles require a temperature slightly lower than the rest of the body to produce healthy sperm. Varicocele disrupts this delicate balance in several ways.
The pooling of blood increases scrotal temperature, which directly interferes with sperm production. Over time, this heat stress damages the cells responsible for spermatogenesis. Varicocele also causes reduced oxygen supply and accumulation of metabolic toxins, further impairing testicular function.
As a result, men with untreated varicocele may experience low sperm count, poor sperm motility, abnormal sperm shape, or a combination of all three.
Can Varicocele Cause Low Sperm Count?
Yes, varicocele is one of the leading reversible causes of low sperm count. Numerous clinical studies have confirmed a strong association between varicocele and reduced sperm concentration.
However, not every man with varicocele will have fertility issues. The impact depends on factors such as the grade of varicocele, duration of the condition, age, and overall testicular health. Higher-grade varicoceles and long-standing cases are more likely to affect sperm count significantly.
Symptoms That May Indicate Fertility Impact
Many men remain unaware of varicocele until fertility testing is done. Still, certain signs may indicate its effect on reproductive health. These include a dull ache or heaviness in the scrotum, discomfort after prolonged standing, visible or palpable enlarged veins, and unexplained infertility despite regular unprotected intercourse.
Low sperm count is often discovered during semen analysis rather than through physical symptoms alone.
Does Treating Varicocele Improve Sperm Count?
In properly selected patients, treating varicocele can significantly improve sperm parameters. Studies show improvement in sperm count, motility, and morphology within three to six months after treatment, as this is the natural sperm production cycle.
Improvement is more likely in men who have abnormal semen parameters before treatment and a clinically significant varicocele. Early intervention often leads to better outcomes compared to delayed treatment.
Modern Approach to Varicocele Treatment
Traditionally, varicocele was treated with open or laparoscopic surgery. Today, minimally invasive, image-guided treatment has transformed patient outcomes.
Varicocele embolization is a non-surgical procedure performed by an Interventional Radiologist. It involves blocking the faulty veins from inside using tiny coils or medical agents, redirecting blood flow through healthy veins. The procedure does not require general anesthesia, stitches, or long recovery periods.
At Expert IR Clinic, Dr. Santosh Patil evaluates varicocele with advanced imaging and offers evidence-based embolization treatment tailored to each patient’s fertility goals.
Benefits of Non-Surgical Varicocele Treatment
Non-surgical embolization offers several advantages for men concerned about fertility. It preserves testicular tissue, avoids surgical scars, and allows faster return to daily activities. Importantly, it treats the root cause—abnormal venous reflux—rather than just the visible veins.
For men planning conception, minimal disruption to hormonal balance and testicular function is a key benefit.
Can Lifestyle Changes Help Alongside Treatment?
Lifestyle measures such as maintaining a healthy weight, avoiding prolonged heat exposure, quitting smoking, and reducing excessive alcohol intake support overall sperm health. However, lifestyle changes alone cannot correct the abnormal veins responsible for varicocele.
They should be viewed as supportive measures rather than definitive treatment.
When Should Men with Varicocele Seek Medical Advice?
Not every varicocele requires immediate treatment. Medical consultation is recommended if a man has low sperm count, infertility lasting more than a year, scrotal pain, testicular shrinkage, or worsening semen parameters over time.
Early evaluation helps differentiate cases that need monitoring from those that would benefit from timely intervention.
Frequently Asked Questions (FAQs)
No. Not all men with varicocele experience infertility. Fertility impact depends on the grade of varicocele, duration, age, and overall testicular health. Higher-grade or long-standing varicoceles are more likely to affect sperm count.
Varicocele causes increased scrotal temperature, reduced oxygen supply, and buildup of toxins around the testicles. These factors damage sperm-producing cells, resulting in low sperm count, poor motility, and abnormal sperm shape.
Yes. In men with abnormal semen parameters, varicocele treatment often improves sperm count and quality within three to six months. Improvement occurs as new, healthier sperm are produced after correcting abnormal blood flow.
No. Varicocele can be treated without surgery using minimally invasive embolization. This image-guided procedure blocks faulty veins from inside, restores normal blood flow, and avoids surgical cuts, stitches, or long recovery.
Sperm parameters usually begin improving within three months, with continued improvement up to six months or longer. This timeline matches the natural sperm production cycle.
Conclusion
Varicocele is a common but often overlooked cause of low sperm count. The good news is that it is one of the most treatable causes of male infertility when identified early and managed correctly.
If you or your partner are facing fertility challenges, timely evaluation can make a meaningful difference. With modern, non-surgical solutions available today, men no longer need to delay care due to fear of surgery or long recovery.
Under the expert guidance of Dr. Santosh Patil at Expert IR Clinic, patients receive precise diagnosis and advanced interventional care focused on restoring fertility, preserving testicular health, and improving long-term outcomes.